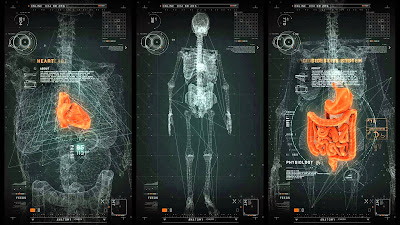
Healthcare informatics is a term describing the acquiring,
storing, retrieving and using of healthcare information to foster better
collaboration among a patient’s various healthcare providers. Health
Informatics plays a critical role in the push toward healthcare reform. Health
informatics is an evolving specialization that links information technology,
communications and healthcare to improve the quality and safety of patient
care. Health informatics applies informatics concepts, theories, and practices
to real-life situations to achieve better health outcomes. This includes
collecting, storing, analyzing, and presenting data in a digital format. The tremendous growth in the health
informatics field was spurred in large part by the acceleration of electronic
health record (EHR) adoption brought about by the Centers for Medicare and
Medicaid Services' "meaningful use" incentive program. As providers move quickly to embrace EHRs,
which are designed to store and share information from all providers involved
in a patient’s care, health informatics specialists will continue to be in high
demand as healthcare facilities implement new systems, upgrade existing
databases and work toward achieving the three stages of “meaningful use.”
Kuehnl-Cadwell, J. (2010). Use the right tool for the right job. Retrieved from www.datawisesolutions.com/database-vs-spreadsheet.shtml
Mancuso, M. (2014). Collaborating our way into interoperability. Health Management Technology, 35, (6), 24.
For more information on healthcare informatics click here
Electronic Health Records and Meaningful Use
Today, technology seems to have a part in every aspect of
life. Everyone has a smart phone or a
tablet. People can’t seem to live
without the internet. This applies to
health care as well. This informatics
class has taught me so much that I didn’t know about in regards to the
importance of technology in the healthcare setting. Electronic health records are a huge part of
the healthcare world. Electronic health
records or EHRs in the United States is becoming more and more prevalent. Adoption of EHRs has been increasing at about
3-6% per year (Jha, 2010). EHRs are
improving the way that patients are cared for and causing decision making to be
easier for providers. There are 3 different stages of to implementing meaningful
use. In 2015 the Centers for Medicare
and Medicaid Services issued a new rule for the EHR incentive program to align
Stage 1 and Stage 2 objectives and measures with the long-term proposals for Stage
3, to build progress toward program milestones, to reduce complexity, and to
simplify providers’ reporting. These
modifications would allow providers to focus more closely on the advanced use
of certified EHR technology to support health information exchange and quality
improvement (Center for Medicare and Medicaid Services, 2016).
For more information, on meaningful use click here
Interoperability
Now
that the clinicians are connected, the next step is to facilitate better care
through technology. There are a great number of "interoperability
solutions" available in the market today. Organizations have proposed a
spread of solutions that can serve as a translator between two or three
different types of patient records. But this approach is not enough. Instead,
the industry needs to fully embrace a set of open standards to create the
structure needed to drive innovation in healthcare technology, so that new
tools and technologies can help clinicians provide better care for their
patients (Mancuso, 2014). With broader standards, EHRs can be shared securely
and enable clinicians to access and even analyze data more easily and more
thoroughly.
Data Mining
In
a typical work day, nurses use technology all the time. A new type of technology is called data
mining. Data mining is a newer
generation approach to data analysis and knowledge discovery that has grown out
of the need to derive meaningful information from the massive amounts of
high-dimensional data that have been produced and stored over the past decade
(Berger & Berger, 2004). Data mining
is being used for research purposes but can be utilized for everyday practice as
well. The technology is being used for analysis, modeling, and prediction in a
variety of scientific disciplines. It is
also used for cataloging and classifying.
Data mining is defined as the semiautomatic exploration and analysis of
large quantities of data in order to discover meaningful patterns and rules
(Berger & Berger, 2004).
Databases
Technology is a huge part of the healthcare system and helps
with the care of patients. Databases,
particularly, are a great resource for nurses and other health care
professionals to utilize in order to keep our patients safe and to give them
the best quality of care possible.
Databases are used by everyone, from doctors to care facilitators. The use of health IT has long been
recommended as a strategy to facilitate cost effective, high-quality, and safe
patient care (Dykes & Collins, 2013).
According to Kuehnl-Cadwell (2010), databases are used to collect,
manipulate, filter and report on various kinds of data. Databases can help nurses find pertinent
information fast and easy.
Reflection
All
of these areas of technology are extremely important to nursing and nursing
leadership. These topics should be taken
seriously and fully understood by leadership.
Technology is not going away; it’s only going to get more
prevalent. It’s crucial for the
application in the healthcare setting to be understood and implemented. These past five weeks have shown me the importance of healthcare informatics and that it is so much more than just "computer stuff." I enjoyed working with the different programs to create presentations. I enjoyed Prezi the most and found it most helpful. I am glad that I have been exposed to such programs and plan on using them in the future. Healthcare informatics is a growing field, and it is essential that we as nurse leaders embrace it and utilize it to our full potential.
References
Berger, A.M. & Berger, C.R. (2004). Data mining as a tool for research and knowledge development in nursing. Computers, Informatics, Nursing, May/June, 123-131.
Dykes, P. & Collins, S., (2013). Building linkages between nursing care and improved patient outcomes: The role of health information technology. The Online Journal of Issues in Nursing, 18, (3).
Jha, A.K. (2010). Meaningful use of electronic health records: The road ahead. Journal of American Medical Association, 304, (15). 1709-1710.